What Goldilocks Can Teach Us About Chronic Pain
Hint: it's all about persistence.
Recently, I was on campus at the University of Kansas in Lawrence, Kansas. We just finished watching our son receive his Master’s diploma in Architecture, where he was “hooded”. A faculty member places a hood over his head and around his neck. It looked more like a scarf to me, but maybe they had it rolled up.
We were outside taking pictures at selected locations on campus before going out for a celebration dinner with architecture roommates, classmates and their families. I scanned my phone for anything new and time-sensitive.
Boom — notification from the Mayo app.
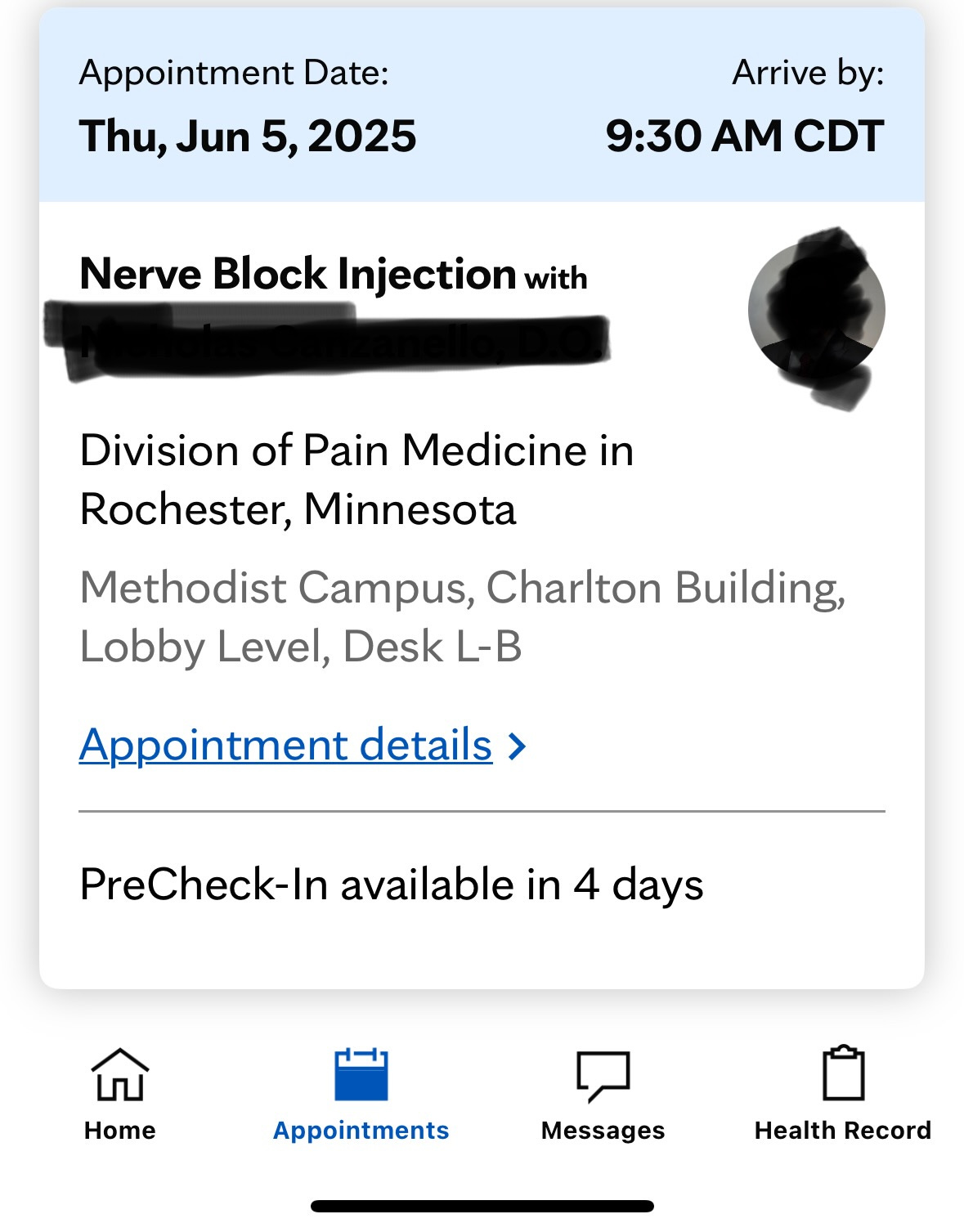
My nerve block was scheduled for Thursday, June 5th. What? That was quick, and the date is coming up quickly — just under 3 weeks away.
How did we get here, how is Goldilocks involved and how did persistence play a role?

Insistence on New Solutions
On May 6, my pelvic floor pain hit an all-time high that I didn’t know could be achievable.
Like the other 10/10 days, it felt like knives stabbing me in an already naturally sensitive area, knives stabbing over and over.
This time, the stabbing took no breaks. I couldn’t walk to my bed from the master bathroom.
My bar of what constitutes a pain level 10 was raised. (Are you kidding me? How could it possibly get any worse? But it was. How in the world can I live like this?) I never know when it’s going to strike.
It is literally stripping away my life as I know it. I started to feel defeated.
Finding the right treatment for this chronic pelvic floor pain feels like Goldilocks tasting the porridge — too hot, too cold, never quite right. And we can never quite find the right treatment to solve my pain.
After re-reviewing Mayo’s write-up from last October, the doctor concluded that if none of these tactics work, we might consider trying a nerve block.
What is a Nerve Block?
A nerve block is when a medication is injected into a nerve and you basically feel nothing in that area until it wears off.
After one of my foot surgeries about 7 years ago, the doctor told me they had done a nerve block during the surgery to help with immediate post-surgical pain. He warned me to be really careful with my right leg until it wore off (another 5-6 hours) as I was feeling nothing from top to bottom on that leg.
I could inadvertently turn the leg in an awkward direction without even realizing it, while the nerve block was still active. From that experience, knowing how powerful a nerve block can be, I became excited about what it could mean for this pain. There are other nerve block types that can last longer than 5-6 hours. They can last months. (Imagine, the pain could be blocked entirely!)
Medication Option
The other option I wanted to pursue is one that my dermatologist recommended: a low dose of a medication used to treat alcoholism. This med blocks the pain / nerve receptors — and it’s been found to stop pelvic floor pain 20% of the time. I locked onto these two approaches and became determined to try one or both of them.
I honestly thought the medication one would be the easiest to accomplish, but I pursued both equally because… who knows?
Mayo pushed back on writing a script for the medication. Their stance from the beginning has been that they will determine the plan and they want my local team to execute.
Dermatology to the Rescue?
A new member of my local team, my dermatologist, made the suggestion for the medication when I threw this new and random question at him during a regular 6-month check-in. (Hey, Doc, uncomfortable question time: I’ve heard that skin issues can be involved in solving pelvic floor pain issues.)
He seemed very excited to address a non-routine question and he gave me a few ideas, including this medication one. He also rightfully suggested taking this back to Mayo, since they are overseeing the case, and that if they approved, he could write the script.
When I circled back to him, with Mayo’s consent, he was no longer willing to own this approach. (Persistence applied #1 - Are you kidding me?)
A Dead End… For Now
After more questioning, he said he could prescribe for the “testing phase,” but that the doctor treating the underlying issue should really own the script. (Persistence applied #2 - Ok, that makes a little more sense, but why not just own the whole thing? Instead, this will make this more complicated for me to execute.)
I do not yet have a doctor outside of Mayo who is agreeing to take ownership of the overall issue, so this idea is currently at a dead end until I apply more persistence elsewhere.
Nerve Block It Is
Taking me by surprise, the nerve block idea has made more traction than the medication.
Knowing that Mayo would default to wanting my local team to execute, I thought through how this could work. Pain Management is the department that executes nerve blocks.
During a previous iteration of this chronic pain issue, I saw a local pain management specialist. It took 5-6 months to get an appointment and that was just for a consult. After that, the nerve block would need to be scheduled.
With my primary Mayo doctor out of the office for most of May, after my persistent messages and calls, the on-duty doctor of the day submitted an order for me to get a nerve block. (Persistence applied #3 - Ok, an order was submitted. This feels like progress… yay!)
I did a double-take at my computer screen …
displaying the Mayo online patient portal message stating a nerve block was ordered. Ok, but how long would it take to get on their schedule?
Amidst all this chaos, we are celebrating in a joy-filled household for our son’s Master’s graduation. We had a long 4-day event schedule in Lawrence, Kansas. It was smack in the middle of these events that I caught the notification on my phone stating that the nerve block was scheduled. And, at the time, it was only 3 weeks away!
Schedule me for any date, just schedule me. Oh, just not THAT date!
I wanted to jump for joy, but jumping is not in the cards for me with this pain. Also, I had a lot of questions.
The Nerve Block… And the DC Trip Collision
At the top of the list is the fact that I am supposed to travel to Washington, DC, for my annual Alzheimer’s Forum trip on Friday, June 6. Would I be able to go to Rochester, Minnesota, for this procedure on June 5 and travel the next day to DC?
Would having a nerve block the day before the start of this trip potentially interfere with my ability to travel or to be able to keep up (even though my ability to keep up is already at risk with the existing pain)? Would it be any worse than it already was going to be?
It should be easy enough to get answers to questions about my scheduled procedure, right? Turns out, no. There is an awkward gap when one department submits the order for a procedure and it’s another department that schedules it.
Not a Patient Here, No Questions Allowed
If I’m not an established patient in the Pain Management Department, I'm unable to send a message via the Mayo online portal, which is typically easy to do. Ok, so I called to get my questions answered. (Persistence applied #4 - It was a relief to be able to talk to a person in Pain Management.)
The Pain Management rep seemed bound by the rules. However, he took down the questions he could not answer so he could send them to someone who could answer them.
He made a point of telling me that I still might not hear back though, as there is no process for anyone to reply to someone who is not an established patient in the Pain Management Department. (Persistence applied #5 - How frustrating! Rather than help a suffering patient, this guy was more interested in adding to the notes, telling me that I might not get a response since I’m not an established Pain Management patient.)
While I had a ton of questions, the top couple of questions were about traveling the day of and the day after the nerve block.
For Goldilocks, the bears’ chairs were either too big or too small. She could not find just the right fit. Would that be the case with this new, seemingly silver bullet solution?
Have Nerve Block, Will Travel
It turns out it’s fine to travel the same day, which would be needed for me to get home on time on Thursday to still make my flight on Friday.
Also, nerve blocks have variable timing in terms of how long it takes for them to take effect. It could be immediate. It could be hours or days.
Many of my questions were answered via a portal response message, however, I still need clarification on two items to know that it is worth it to travel to Rochester:
I have an existing nerve stimulator in my right hip for an unrelated issue. There are wires that touch some of my nerves and lead back to the stimulator. Does the doctor performing the nerve block need to know where these wires are to avoid them?
1b. And I’d like to confirm that they still believe the nerve block is a good idea, even with the existing nerve stimulator that I have.
The order was written to put the block on the pudendal nerve. At first glance, that feels like the right nerve to block. But is it?
Based on my physical therapist’s experience working with me, there are three other nerves that are better candidates than the pudendal nerve, with the gentiofemoral nerve being her #1 pick. (Numbers 2 and 3 are the ilioinguinal nerve and the hypogastric nerve.)
Questions That Still Need Answers
I made yet another phone call to the Pain Management Department at the Mayo Clinic. I got someone completely different this time, and that made all the difference. (Persistence applied #6 - What a breath of fresh air, to feel validated and get the help that I need!) She apologized for the fact that a pre-procedure phone call had not been scheduled yet and she immediately set one up for the next business day, which at this point was Tuesday, May 27. I’ll still have over 1 week’s notice to plan the trip, if Rochester is a go.
Six times!
I had to be persistent 6 times to make something meaningful happen.
And I’m not quite there yet, but I do feel good that I will get the necessary answers on Tuesday and that the nerve block will be a go. (Always the optimist.)

Persistence and the Three Bears
The moral of this story is to be persistent… like Goldilocks. I don’t think anyone is more persistent than that girl who shacked up with three bears. Whether the bed was too big or the chairs were too short, she spoke her mind, all in the face of bears. Bears are known for eating people. Ok, I know this is a fairy tale, but those tales are there to teach us lessons, so bear with me on this.
I’ll let you all know if this fairy tale has a happy ending or if I’m still fighting bears! Stay tuned.
Sign up now to receive future newsletters directly in your inbox for free. Or upgrade to paid for more reader benefits.



What an amazing story…and not a fairytale.
Julie,
Your words carry such tender strength. Even in your pain, you show up with a heart full of honesty—and to me, that’s the opposite of unpredictable.
That’s devotion. That’s grace.
I see the persistence in your search for healing and relief, the way you keep reaching for light even when the path is steep and uncertain. Life has its own rhythms, and yours is calling for bravely pressing for solutions, self-care, and trust in yourself.
I’m here, gently cheering you on as you find your way back to steadier ground and hopefully soon, a pain-free life. You’re not alone, and you are courageous and supported—more than you know.